Family caregiving—whether it is elder care or caring for an otherwise disabled individual—involves offering physical, emotional, and logistical support to a loved one who requires…


Family caregiving—whether it is elder care or caring for an otherwise disabled individual—involves offering physical, emotional, and logistical support to a loved one who requires…
It’s not uncommon for family caregivers to feel like they are invisible. In the family caregiver role, they continually serve their loved one. The needs…

As I meet caregivers across the country, they tell me, time and again, how their lives have changed. Many changes involve the tasks of care…

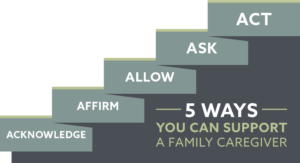
When I first introduced the model of caregiver resilience, I explained that this is a learning model. In today’s installment of the series of blog…

Family caregivers often report that caring for a loved one is among the hardest things they’ve ever done. Until you’ve assumed the responsibilities of caregiving,…

Caregiving changes relationships. While this can be disorienting and unwelcome, it’s among the most important things for caregivers to realize as they seek to meet…